Middle-toe joint pain can result from various factors, often affecting daily activities and mobility. One common cause is arthritis, which leads to inflammation and stiffness in the joint. This condition can be a result of wear and tear over time or due to an autoimmune disorder. Another cause of this type of pain is a bunion, where a bony bump forms at the base of the big toe, as the result of misalignment of the toes. Trauma or injury, such as a sprain or fracture, can also lead to pain in the middle toe joint. Symptoms of middle toe joint pain include swelling, redness, and tenderness in the affected area. The pain typically worsens with movement, and it may become difficult to walk or wear shoes. In some cases, the joint may become stiff, limiting flexibility. If you have toe pain, it is suggested that you schedule an appointment with a podiatrist who can determine what the cause is, and offer viable treatment solutions.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Foot Health Center of Merrimack Valley. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
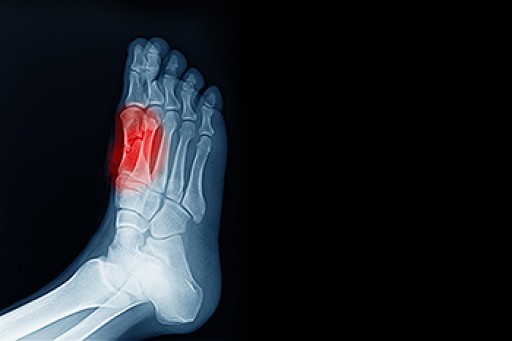
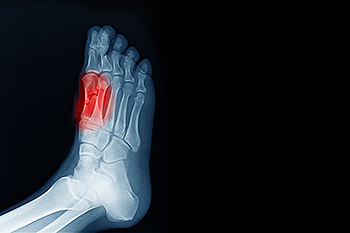
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact one of our offices located in North Andover, and Tewksbury, MA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.